Urinary Incontinence
Urinary incontinence is described as involuntary or accidental leakage of urine. While bladder leakage is not a serious or life-threatening condition but it can significantly impact ‘quality of life’. It affects up to 40% of Australian women. Approximately 65% of women have some form of bladder leakage but only 30% seek help from health professionals. Social embarrassment and normalising bladder leakage as part of childbirth and ageing process are the main barriers to women getting assistance. This condition can be treated with conservative management or surgery depending on the cause of bladder leakage.
What are the types of urinary incontinence?
Stress urinary incontinence – involuntary urinary leakage during activities such as coughing, sneezing, laughing or exercising
Urge incontinence – involuntary urine leakage preceded by bladder urgency (strong desire to pass urine/needing to rush to toilet). The symptom may be associated with urinary frequency (going to toilet frequently) or nocturia (waking up at night to pass urine)
Mixed urinary incontinence – combination of both stress and urge incontinence occurred concurrently. Some women have one symptom worse than the other
Overflow incontinence – insensible urine leakage that is not associated with any activities or urinary urgency. Patient may have no desire or sensation to pass urine and may have sensation of incomplete bladder emptying. This may be due to urinary retention resulting in a overdistention bladder injury eventually urine overflow.
Coital incontinence – Involuntary urine leakage during sexual intercourse. It may occur during penetration (which may be associated with stress incontinence) or during orgasm (this may be associated with an overactive bladder)
Other types of incontinence
Urogenital fistula – abnormal connection between your bladder/ureter/urethra with vagina. Patients with this condition may have persistent urine leakage/trickle that is not associated with any activities or urinary urgency.
What causes urinary incontinence?
Pregnancy and childbirth are the main causes of urinary incontinence. Ageing and menopause, obesity and others are also contributing factors to urinary incontinence.
How can this be assessed?
The initial clinical assessment will take place during the consultation including an internal exam and a urine test to exclude urinary tract infection.
You will be given a 3-day bladder diary to record your daily fluid intake, voided urine volume and any bladder leakage episodes to assist with identification of type of urinary incontinence.
If your bladder leakage does not improve with non-surgical approach or the cause remains unclear, advanced bladder testing may be required (see Urodynamics & Cystoscopy)
Non-surgical approach to urinary incontinence
Weight loss (combined dietary modification and exercises)
Clinical research has demonstrated improvement in urinary incontinence by 50% with weight loss of 5-8% of your current weight.
Pelvic floor physiotherapist
Good quality evidence has suggested that women who had intensive supervised pelvic floor muscle strengthening are more likely to have less urine leakage, cure of incontinence and improvement in quality of life compared to no treatment. A concurrent bladder training may take place to manage your urge incontinence.
Continence pessary
May provide additional support to your water pipes to minimise bladder leakage.
Fluid intake modification/reduce caffeine intake
May improve your urinary urgency and urge incontinence by limiting the bladder irritants.
Avoid or treat constipation
May improve your bladder emptying function, and reduce chances of developing urinary incontinence.
Medications
Can be used if you have overactive bladder symptoms or urge incontinence symptoms (see Overactive bladder section)
Percutaneous tibial nerve stimulation (PTNS)
A non-drug & non-surgical management of urge incontinence
Effective office-based neuromodulation delivering small electrical impulses through tibial nerve (behind your shin bone) to restore your bladder function. During the procedure, an acupuncture needle will be placed near your ankle and connected to an external stimulator.
A 30 minute, 12 week treatment plan is required to achieve desired treatment response. Maintenance can be achieved with 30 mins monthly treatment.
This treatment can be used alone or in conjunction with other medications with minimal side effects
Surgical options for female stress urinary incontinence
Synthetic mid-urethral sling
A retropubic sling involves the insertion of a permanent synthetic sling through a small vagina incision and passed through behind the pubic space with a small exit incision on each side of the pubic bone.
This is the gold standard treatment for stress incontinence with well-established long-term efficacy and safety
This procedure can be done alone or in conjunction with prolapse surgery.
Burch colposuspension
This mesh-free surgery involves placement of sutures on each side of the mid-urethra (water pipe) and into the ligament of the pubic bone (Cooper’s ligament) to re-establish the urethral support using your own tissue
This is an alternative surgical option for women who wish to avoid mesh use. The surgery can be achieved through a laparoscopic or robotic surgery
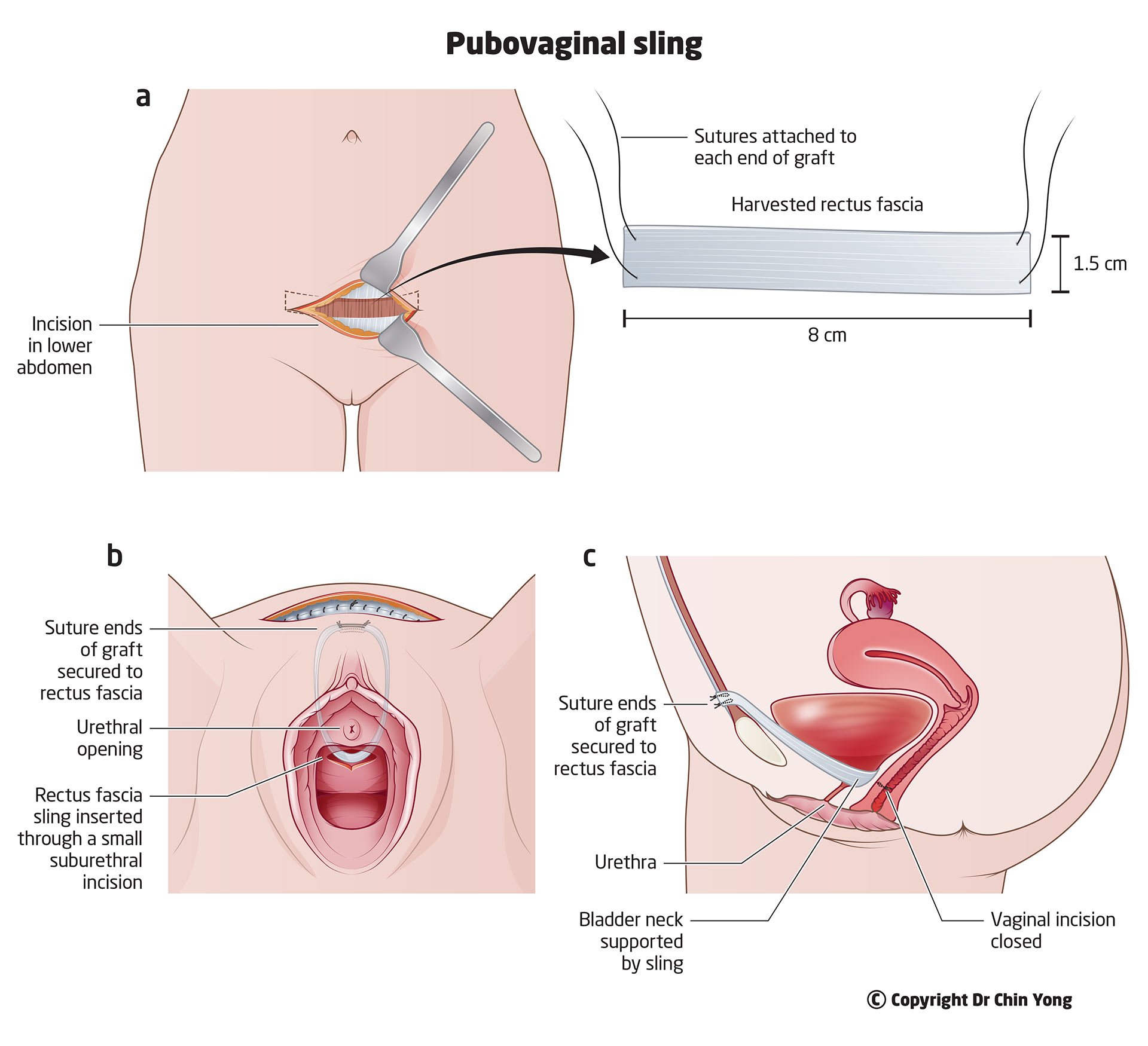
Pubovaginal sling
Another alternative mesh-free surgery option uses your own tissue involving an abdominal incision (slightly smaller than Caesarean section scar) to harvest a piece of sling
Once the sling is harvested, it will be introduced in a similar manner as midurethral sling and secured onto rectus sheath.
The recovery may be slightly longer than the first two surgical options due to larger abdominal incision
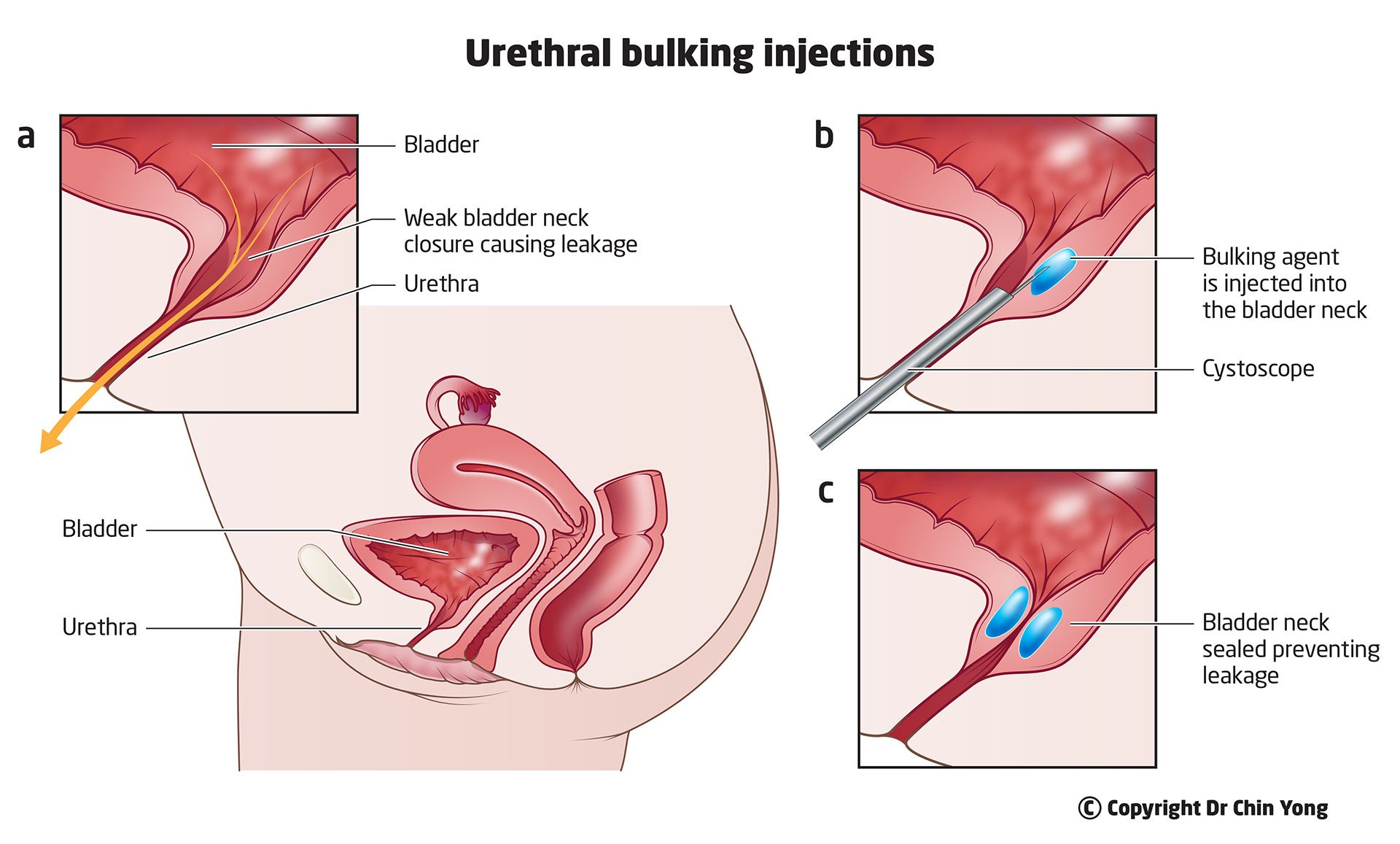
Urethral bulking injections
A long acting urethral filler (consist of 97.5% of water & 2.5% hydrogel) to bulk up the water pipe preventing urine leakage
The procedure will be performed under direct vision using a small scope into urethra
This is a good surgical option for patients who wish to have a temporary solution for the treatment of stress incontinence. Not suitable for more invasive options as above due to medical conditions or a rigid/scarred urethra from previous surgery
The surgery may be repeated if the urinary incontinence recurred
Surgery options for urge incontinence
Botox injections into the bladder
An advanced therapy option for patients who failed to respond to oral medications for overactive bladder and urge incontinence
This day procedure involves 20 small injections of botox into the bladder under direct vision using a cystoscopy
The Botox effects last approximately 6-9 months and top up can be offered if urge incontinence reoccurs.
Most common adverse effects include urinary tract infection and urinary retention requiring short-term intermittent self-catheterisation.
Sacroneuromodulation (SNM)
SNM may be recommended for women who failed to respond to oral therapy for overactive bladder and urge incontinence
Thought to work by stimulating the sacral nerves in your lower spine that subsequently send signals to brain to restore your bladder function
It can also be used for treatment of faecal incontinence and non-obstructive urinary retention
This is a two-staged procedure:
Stage 1 involves insertion of an electrode into your lower back under radiological guidance in the operating theatre and connected to temporary external stimulator. A permanent implantable pulse generator (IPG) can be inserted when at least 50% improvement in bladder symptoms been observed in the 7 days bladder diary.
Stage 2 procedure involves insertion of IPG through a small skin incision above your hip bone under general anaesthesia
Useful Websites