Vaginal Prolapse
Vaginal prolapse is a common condition that can be caused by a bulging and herniation of one or more pelvic organs, such as the bladder, uterus or bowel, into or out of the vagina. This is a not life-threatening condition but can have impact on quality of life. Most women will have improved symptoms with expert management either conservatively or surgically.
Is it common for women to have prolapse?
Affects up to 50% of women following childbirth and 40% of women may develop symptoms. Around 10-20% may require surgical correction of the prolapse at some stage in their life.
What causes pelvic organ prolapse?
Prolapse results from weakened or damaged pelvic floor ligaments, muscles, nerves or the tissues responsible for the supporting pelvic organ. This can happen after:
Pregnancy & childbirth – independent risk factors leading to a weakening or damage to pelvic organ support. The risk increases exponentially with forceps delivery.
Ageing & menopause – altered tissue quality, strength and integrity with age
Prolonged, excessive pressure on pelvic floor muscle such as obesity, chronic constipation, heavy lifting and straining
Inherited connective tissue disorders such as Marfan’s Syndrome or Ehlers-Danlos syndrome
What are the symptoms suggestive of pelvic organ prolapse?
Heaviness or dragging sensation in the vagina or lower back
Vaginal lump or bulge
Discomfort during intercourse
Bladder symptoms: slow urinary stream, incomplete bladder emptying, urinary urgency, frequency or urinary incontinence
Bowel symptoms: difficulty or incomplete bowel emptying, assisted bowel emptying using finger to press onto the vagina bulge
Non-surgical treatment options
Vaginal pessary
A removable device that is inserted vaginally to reduce vagina bulge. This device may improve the bulge symptoms but does not reverse pelvic organ prolapse.
Can be considered if a patient wishes to avoid or delay surgery, has not completed child bearing, unfit for surgery due to medical conditions, treatment of prolapse during pregnancy.
Dr Yong offers different types of pessary. Please contact our room for further information.
Pelvic floor physiotherapy
Intensive, supervised pelvic floor muscle training has been proven to improve prolapse symptoms but does not reduce the severity of clinical prolapse.
Dr Yong collaborates with various pelvic floor physiotherapists in Melbourne as a first line treatment of pelvic organ prolapse symptoms. A referral can be made to your local physiotherapist if required.
Surgical treatment for pelvic organ prolapse
Surgery can be considered when the prolapse symptoms failed have to improve with conservative therapy or for those who declined non-surgical management.
Uterine conservation surgery or hysterectomy?
A Hysterectomy may not be necessary for the treatment of pelvic organ prolapse. However, a careful clinical evaluation will be required before considering uterine conservation surgery or a hysterectomy. This surgery can be achieved by a laparoscopic (key hole), robotic or vaginal approach. A laparoscopic approach can be considered if a women wishes to have their tubes removed. The ovaries are not usually removed during a hysterectomy for prolapse unless indicated e.g. family history of ovarian cancer or BRCA gene positive.
What are the prolapse surgery options?
Vaginal surgery
Vaginal hysterectomy – removal of uterus for treatment of advanced uterine prolapse or a lack of desire to conserve uterus
Vagina wall repair – reinforcement of weakened pelvic organ support on anterior (front) or posterior (back) vagina wall using sutures
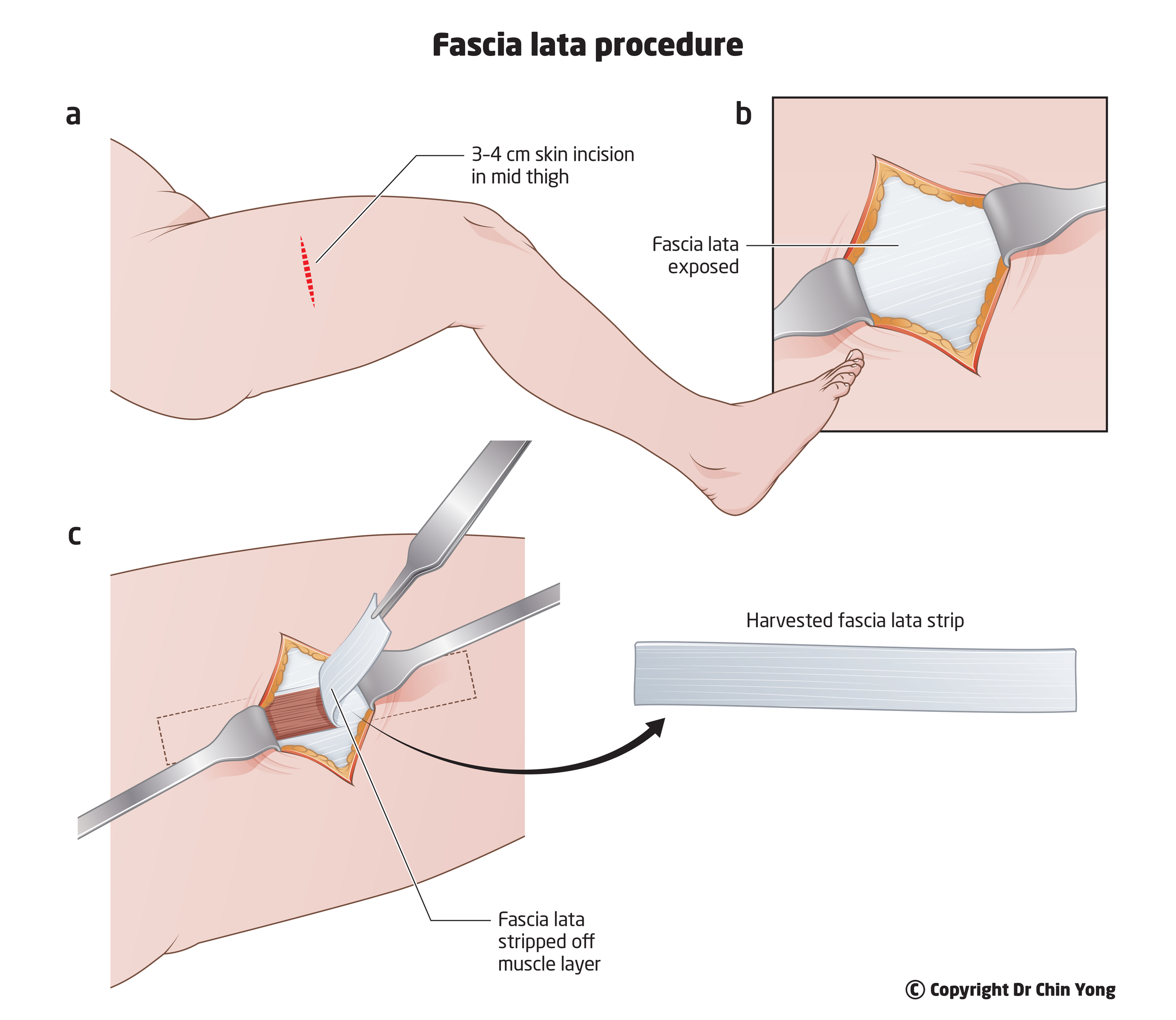
Vaginal repair reinforced with autologous fascia lata – As of January 2018, TGA withdrawn all synthetic or biological grafts for transvaginal prolapse repair in Australia. Fascia lata can be considered for patients with advanced or recurrent pelvic organ prolapse
Vaginal sacrospinous colpopexy (hysterectomy) or hysteropexy (uterine conserving) – lifting of the vagina apex (vagina vault) or uterus using sutures anchoring it onto the sacrospinous ligament.
Colpocleisis – surgery to close off the vagina by sewing the front and back walls of the vagina together using sutures keeping the uterus in place. This is a simple and quick procedure suitable for women who are no longer sexually active.
Laparoscopic (keyhole) or robotic surgery
Uterosacral ligament uterine suspension or colpopexy (post hysterectomy) – mesh-free surgery
Involves re-suspension of the uterus to the uterosacral ligaments using sutures. This is a native tissue uterine preservation prolapse surgery option
Suture colpopexy is utilised for women who have had a hysterectomy or a concurrent hysterectomy as part of the prolapse treatment. This surgery involves re-suspension of roof of vagina to the uterosacral ligaments using sutures
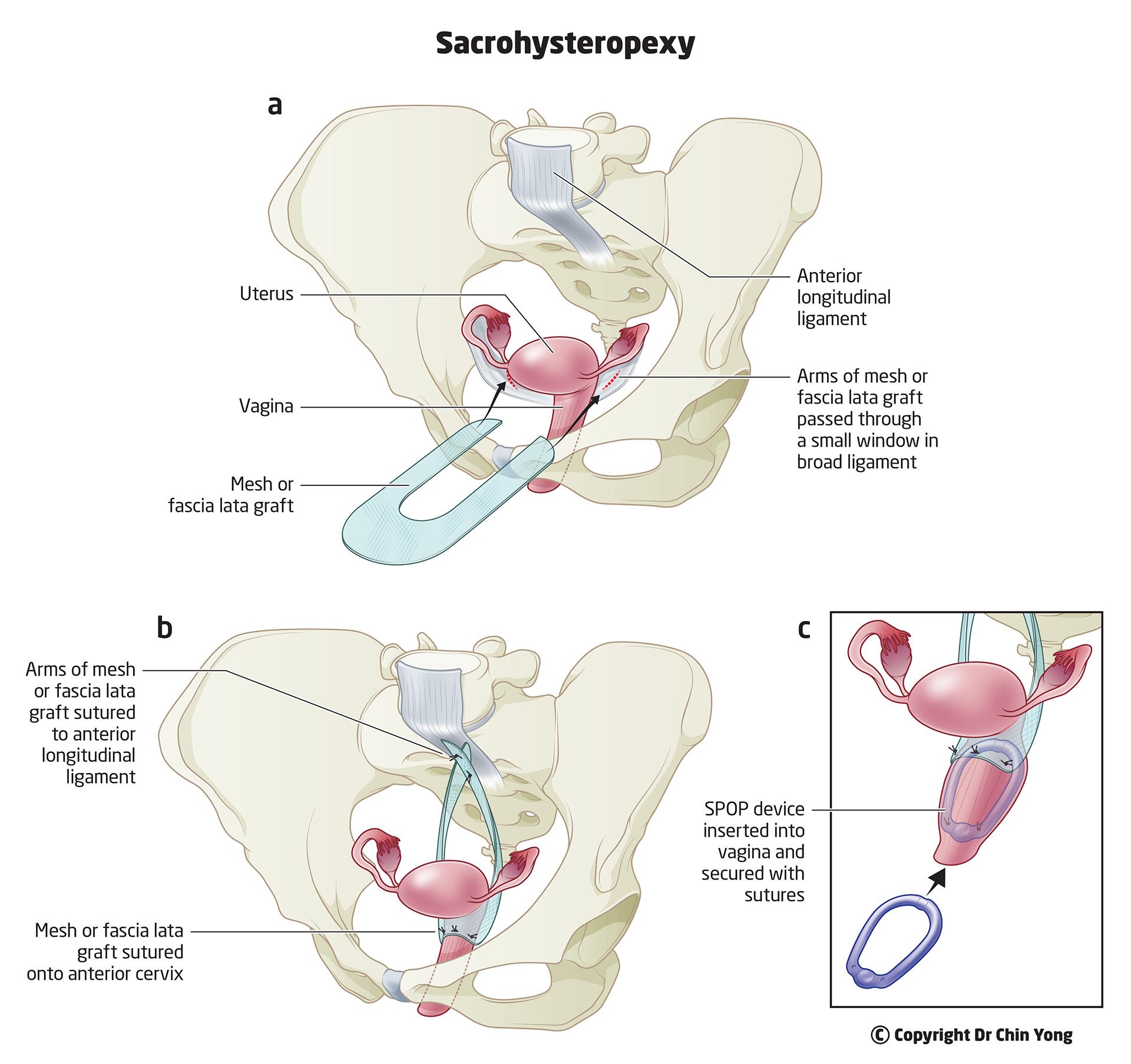
Sacrohysteropexy
Use of synthetic mesh to suspend the uterus from the front of sacrum (tail bone) to provide support for the uterus and upper vagina. Autologous fascia lata can be considered for women who declined pelvic mesh use. A concurrent vaginal repair may be required.
This surgery is usually reserved for women with advanced uterine prolapse who wishes to conserve their uterus or when previous uterus support surgery has failed.
Sacrocolpopexy
Involves suspension of upper vagina after hysterectomy using synthetic mesh (or fascia lata) from the front tail bone. A concurrent vaginal repair may be required.
This surgery is usually reserved for women with advanced or recurrent vault prolapse.
Native tissue fascia lata surgery
Fascia lata is a deep strong connective tissue of the thigh. This fascia can be harvested and utilised to reinforce weakened tissues during pelvic organ prolapse or stress incontinence surgery.
Fascia lata can also be used as pelvic mesh replacement if women wishes to avoid synthetic pelvic mesh use.
What are the possible surgical complications?
General surgical risks associated with any form of surgery include: anaesthetic, excessive bleeding, infection (e.g. surgical wound, urinary tract infection), potential venous thromboembolism (blood clots formation in lower leg or lung).
The above risks can be minimised by:
Intravenous antibiotics during and after surgery (usually 24-48 hours) to reduce overall infection risks
Vaginal pack to tamponade potential internal bleeding after vaginal surgery
Administration of blood thinning injections in conjunction with compression stockings/device and early mobilisation to reduce risk of blood clot formation in the legs.
Injury to surrounding structures such as bladder, bowels, ureters, blood vessels or nerves are uncommon. A careful inspection of pelvic structures at the end of key hole surgery (if you are having one) and a cystoscopy (camera into the bladder) will be undertaken to ensure no injuries occurred during the operation.
Bladder emptying problems are common (up to 5%) after pelvic floor surgery and may be higher if incontinence surgery is performed at the same time. An indwelling catheter will be in place for 24-48 hours to allow the bladder to rest. Some women may go home with a catheter for 7 days to provide a longer period of bladder recovery.
New onset of urinary urgency with or without incontinence may occur after prolapse surgery. This can be managed conservatively during the initial recovery phase and may require further management if becoming bothersome.
Painful intercourse can occur after surgery due to scar formation. This problem can be treated with vaginal dilator use and sometimes may require minor surgical revision.
Rare long-term complications such as abdominal hernia, bowel obstruction or adhesions may occur following keyhole or abdominal surgery. Further surgery may be necessary if complication occurs
Pain may occur immediately after surgery but is generally resolved with a few days of pain relief. It is rare for women to experience long-term pain after prolapse surgery. When vaginal sacrospinous hysteropexy or colpopexy is required, some women may experience buttock pain (5-15%), this is usually manageable with oral analgesia.
Whenever synthetic mesh is used during laparoscopic surgery, a small portion of the mesh can be exposed in the vagina (approximately 1-2%). This problem can be treated by using vaginal estrogen therapy or a small vaginal operation to remove the exposed mesh.
Note: This information is intended as a brief guide to pelvic organ prolapse treatment. Dr Yong will be able to provide a more specific advice before making any decision on further treatment. It is advisable that you read all the written information provided before the surgery.
Recovery following prolapse surgery
What to expect after surgery?
You will have a catheter (tube) in your bladder draining urine freely for bladder rest and a vagina pack (similar to a large tampon) to prevent bleeding. The catheter and pack usually remain in place for 24-48 hours depending on the extend of pelvic floor surgery required. A Surgical Pelvic Organ Prolapse (SPOP) device will remain in place for 4 weeks after surgery to provide additional support to the repairs and also promoting recovery. You may experience light bleeding for 1-2 weeks and creamy vaginal discharge from SPOP device use.
Pain or discomfort after surgery
Vagina and lower abdominal pain, or discomfort, is not uncommon and is easily managed with regular pain relief while in hospital. You may experience buttock pain or discomfort after sacrospinous ligament fixation but gradually improve within 1-2 weeks. Occasionally you may also have shoulder tip pain or discomfort following key hole surgery due to residual gas in your abdomen.Prevention of deep vein thrombosis (blood clot)
Compression stockings with a graduated calf compression device will be used in first 24 hours after surgery to minimise the risk of blood clot formation in your leg. You will also be given a blood thinning injection daily. It is advisable that you mobilise as soon as possible after surgery. We encourage you to perform simple leg exercises while in bed to prevent blood clot development (similar to exercises during long haul flight).Bladder and bowel function after surgery
Some women may experience slow urine flow after prolapse surgery. It is not uncommon to have voiding difficulty due to the swelling in vagina. A catheter insertion may be required until bladder function returns to normal. You will be prescribed laxatives (stool softeners) after surgery to prevent constipation. It is important to avoid excessive straining during a bowel motion as it can put pressure on the sutures from prolapse repair.
What type activities that I can do or avoid after surgery?
You may feel more tired or washed out after surgery. Make sure take plenty of rest and listen to your body. Generally, most women will be able to resume their usual daily activities such as walking.
Things to avoid:
Do not exercise or perform heavy lifting (anything more than 5kgs) for at least 6 weeks following surgery.
Swimming and spa pools should be avoided to minimise the risk of wound infection or wound breakdown.
Smoking delays wound healing and increases risk of wound infection. Try to stop smoking if possible.
Do not drive when you are taking sedatives or unable to perform emergency brakes if needed. As a general guide, avoid driving for 1-2 weeks. Some insurance companies place restrictions on driving after surgery. Please check your policy details with the company.
When can I start having sexual intercourse?
It is advisable to avoid sexual intercourse for at least 6 weeks. It may be uncomfortable to initiate intercourse due to anxiety of disrupting the surgical repair or vaginal dryness. Vaginal lubricant can be used if you experienced vaginal dryness.
When can I go back to work?
As a general guide, most people will take 2-6 weeks off work depending on the nature of the job. It may be advisable that you organise a shorter working hours or lighter duties when you first return to work, especially if your job involves frequent heavy lifting or prolonged standing. A medical certificate can be provided to your employer to accommodate your work place requirements.
Useful Websites